Tuesday, June 27, 2006
Ahhhh.... vacation!
I'll be away on vacation until July 5 at a cottage without phone or computer. It will be good to unplug and recharge. See you after the holiday!
In the News: Pomegranate Juice Slows PSA Acceleration Rate After Prostate Cancer Surgery, Radiation
 Newswise (06/27/06) — Pomegranate juice packs a punch on prostate cancer that prolongs post-surgery PSA doubling time, drives down cancer cell proliferation and causes prostate cancer cells to die, according to a study published in the July 1 issue of Clinical Cancer Research.
Newswise (06/27/06) — Pomegranate juice packs a punch on prostate cancer that prolongs post-surgery PSA doubling time, drives down cancer cell proliferation and causes prostate cancer cells to die, according to a study published in the July 1 issue of Clinical Cancer Research.Researchers at the Jonsson Cancer Center at UCLA reported that patients with recurrent prostate cancer who drank pomegranate after surgery or radiation treatment saw their PSA blood content levels double after about 54 months. By comparison, PSA levels in the same patients prior to drinking the daily doses of eight-ounce pomegranate juice accelerated more quickly, doubling their PSA levels in only 15 months.
PSA, or prostate specific antigen, is a protein marker for prostate cancer. The faster PSA levels increase in the blood of men after treatment, the greater their potential for dying of prostate cancer.
“The velocity of the increase in PSA is decreased by 35 percent among those who drank the pomegranate juice,” said Allan Pantuck, M.D., associate professor, Department of Urology, David Geffen School of Medicine, UCLA, and lead author of the paper.
“We are hoping that pomegranate juice offers a novel strategy for prolonging the doubling time in men who have been treated for prostate cancer,” Dr. Pantuck added.
According to the study, sera from patients after treatment yielded a net decrease of almost 30 percent in the numbers of prostate cancer cells raised in culture. Similarly, cultured sera from these patients decreased cell proliferation by 12 percent, compared to cells grown with sera from the men taken prior to initiation of the pomegranate treatment program. In addition, treated sera induced 17 percent more programmed cell death, or apoptosis, than sera from the men prior to treatment.
Additional exploratory experiments conducted by Dr. Pantuck and his colleagues examined antioxidant characteristics of the fruit juice.
“Pomegranate is high in antioxidants, and there is good evidence that inflammation plays an important role in prostate cancer,” he said.
Dr. Pantuck and his colleagues detected a 23 percent increase in nitric oxide sera content from patients after they began their daily pomegranate regimen. These studies were conducted in the UCLA laboratory of Louis Ignarro, Ph.D., the Nobel laureate who contributed key scientific findings to define the role of nitric oxide in health and disease.
As with vitamin C and other antioxidants, ellagic acid – a primary antioxidant in pomegranate juice – works to quench molecules that oxidate, or add oxygen, to cellular and circulatory proteins and fats, altering their biological function.
“By quenching oxidative species with antioxidants, you are basically preserving circulating nitric oxide, so it can have a greater biologic effect,” Dr. Pantuck said. “By decreasing the amount of free radicals, you are probably decreasing the circulating factors that are destroying nitric oxide.”
While their findings on nitric oxide, cell proliferation and apoptosis served as exploratory endpoints, Dr. Pantuck stressed that clinical trials with more precise design are necessary to confirm the biological role the fruit plays in prolonging or preventing recurrence of prostate cancer in men.
“We don’t believe we are curing anyone from prostate cancer,” he said. “In our initial trial, although a third of patients experienced a decrease in their PSA during the study, nobody’s PSA went to zero.
“The PSA doubling time, however, was longer. For many men, this may extend the years after surgery or radiation that they remain recurrence free and their life expectancy is extended. They may be able to prevent the need to undergo additional therapies, such as radiation, hormonal or chemotherapies.”
Dr. Pantuck’s colleagues who contributed to this study included Ignarro, John Leppert, Nazy Zomarodian, William Aronson, Jenny Hong, James Bernard, Navindra Seeram, Harley Liker, Hejing Wang, Robert Elashoff, David Heber, and Arie Belldegrun from the departments of Urology, Medicine, Physiologic Science or Biomathematics at the David Geffen School of Medicine, UCLA. Michael Aviram from the Technion Faculty of Medicine, the Rambam Medical Center, Bat – Galim, Haifa, Israel, also contributed to these studies.
Funding to support these studies came from the Lynda and Stewart Resnick Revocable Trust. The Resnicks are the owners of the POM Wonderful Company. Additional NIH funding (P50CA92131 and IR01CA100938) supported portions of the science conducted in the course of these experiments.
Monday, June 26, 2006
Veggie Hero: Jon Camp
 This week's Veggie Hero is Jon Camp, the hard working outreach coordinator for Vegan Outreach. He has been actively leafleting for Vegan Outreach for four years and has been an employee for about two years. Jon has handed out an amazing 160,000 copies of "Why Vegan" and "Even If You Like Meat" booklets in that time -- mostly at colleges across the nation. He has also distributed more than 80,000 pro-veg booklets for other groups. Jon lives in Takoma Park, Maryland.
This week's Veggie Hero is Jon Camp, the hard working outreach coordinator for Vegan Outreach. He has been actively leafleting for Vegan Outreach for four years and has been an employee for about two years. Jon has handed out an amazing 160,000 copies of "Why Vegan" and "Even If You Like Meat" booklets in that time -- mostly at colleges across the nation. He has also distributed more than 80,000 pro-veg booklets for other groups. Jon lives in Takoma Park, Maryland.Vegetarian or vegan?
Vegan
How long have you been veg*n?
I've been vegetarian for a little over 11 years, vegan for a little over eight years.
What inspired you to go veg?
In the spring of 1995, I took an ethics course at the College of Lake County in Grayslake, Illinois. My professor spent one day explaining what animals endure on factory farms and in slaughterhouses. Moreover, he gave some convincing arguments as to why this should possibly be of moral concern to us. As I'd considered the issue before and always had a sense of empathy for animals, I was convinced and went vegetarian that day. After reading about the issue more, I eventually went vegan.
What's your best story of trying to find veg food?
While I try to be one who dwells on the positive, I've found it quite easy to get vegetarian food about anywhere. During the last two schooI years I've driven around pretty much most of the eastern half of the United States as well as the south, handing out booklets at colleges. I can't remember going hungry once. The amount of vegetarian and vegan food available at mainstream supermarkets and restaurants continues to increase daily.
How do you handle family holiday dinners?
I live far away from most of my family so holiday dinners tend to be by myself or with some fellow vegans. That said, members of my family (some of them veg, some not) are quite respectful of my veganism and I've always found that treating others with a sense of courtesy and kindness is in the animals' best interests.
What's your favorite veg food?
Ethiopian
Do you have a favorite veg book?
As self-promoting as it may sound, I like simplicity and think that Vegan Outreach's "Why Vegan?" and "Guide to Cruelty-Free Eating" make a convincing, succinct case as to why one should adopt a vegetarian diet and how one would go about doing so in a healthy, sustainable manner. If individuals would like a free copy, they can order one here: http://www.veganoutreach.org/starterpack/free-vsp.html
Tofu or tempeh?
I'm a man of frugality and tofu tends to be cheaper.
What did you have for breakfast today?
I started off the morning with a banana and some orange juice, worked out and then throughout the morning, while at my computer, filled my belly up with two bagels (one blueberry with soy margarine, one multigrain with apple butter).
Sunday, June 25, 2006
3ABN Online Vegan Cooking Show
Seventh-Day Adventists have long been on the cutting edge of healthy eating. Today, many followers of this Christian faith are vegans.
3ABN, a international Seventh-Day Adventist cable television station, airs a number of fine vegan cooking programs. "Let's Cook" airs on Tuesday mornings at 8:30 a.m. EST and Thursday afternoons at 2:30 p.m. EST. "3ABN Today" airs at at 9 a.m., 4 p.m. and 10 p.m. EST each Wednesday. "Food For Thought" airs on Monday mornings at 8:30 a.m. EST and Tuesday afternoons at 2:30 p.m. EST. You can watch in real-time online at: http://www.3abn.org/. The recipes are also posted each week.
Now, we just need to get the Food Network on board!
3ABN, a international Seventh-Day Adventist cable television station, airs a number of fine vegan cooking programs. "Let's Cook" airs on Tuesday mornings at 8:30 a.m. EST and Thursday afternoons at 2:30 p.m. EST. "3ABN Today" airs at at 9 a.m., 4 p.m. and 10 p.m. EST each Wednesday. "Food For Thought" airs on Monday mornings at 8:30 a.m. EST and Tuesday afternoons at 2:30 p.m. EST. You can watch in real-time online at: http://www.3abn.org/. The recipes are also posted each week.
Now, we just need to get the Food Network on board!
Saturday, June 24, 2006
Asheville, NC Named One of the Best Veg-Friendly Towns
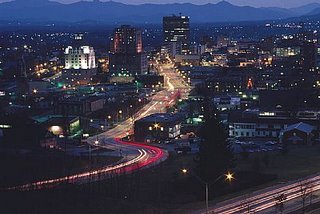 Asheville, my lovely hometown, has been named one of the top 12 "Best Veg-Friendly Places to Live" in the new issue of VegNews!
Asheville, my lovely hometown, has been named one of the top 12 "Best Veg-Friendly Places to Live" in the new issue of VegNews!If you come to visit this veggie paradise, be sure to check out these spots --
The Laughing Seed Cafe -- world famous veg cuisine
Rosetta's Kitchen -- Vegetarian food for Gen-Xers and beyond
Ultimate Ice Cream -- "micro-churned" ice cream, gelato, sorbet (vegan) or soycream (vegan)
Earth Fare -- the nation's third largest health food store chain got started right here in Asheville
Greenlife Grocery -- another great health food grocery
French Broad Food Co-op -- "old school" style health food co-op
In addition, many of our great restaurants offer great veg fare. And be sure to delve into the green wilderness surrounding our city -- Asheville is circled by more than a million acres of national forests!
Friday, June 23, 2006
Ahimsa
 Hinduism is arguably the world’s oldest religion. This venerable tradition has much to teach us, including how to better practice “ahimsa,” or nonviolence.
Hinduism is arguably the world’s oldest religion. This venerable tradition has much to teach us, including how to better practice “ahimsa,” or nonviolence.The late Satgura Sivaya Subramuniyaswami wrote beautifully on this topic in his landmark book, “Dancing with Shiva: Hinduism’s Contemporary Catechism.”
Let’s take a look at a direct quote --
Sloka 69 - Is Vegetarianism Integral to Noninjury?
Hindus teach vegetarianism as a way to live with a minimum of hurt to other beings, for to consume meat, fish, fowl or eggs is to participate indirectly in acts of cruelty and violence against the animal kingdom. Aum.
Bhashya
The abhorrence of injury and killing of any kind leads quite naturally to a vegetarian diet, shakahara. The meat-eater's desire for meat drives another to kill and provide that meat. The act of the butcher begins with the desire of the consumer. Meat-eating contributes to a mentality of violence, for with the chemically complex meat ingested, one absorbs the slaughtered creature's fear, pain and terror. These qualities are nourished within the meat-eater, perpetuating the cycle of cruelty and confusion. When the individual's consciousness lifts and expands, he will abhor violence and not be able to even digest the meat, fish, fowl and eggs he was formerly consuming. India's greatest saints have confirmed that one cannot eat meat and live a peaceful, harmonious life. Man's appetite for meat inflicts devastating harm on the earth itself, stripping its precious forests to make way for pastures. The Tirukural candidly states, "How can he practice true compassion who eats the flesh of an animal to fatten his own flesh? Greater than a thousand ghee offerings consumed in sacrificial fires is not to sacrifice and consume any living creature." Aum Namah Sivaya.
Photo credit: Kauai Aadheenam
Thursday, June 22, 2006
Dressing Up Convenience Food
 Let's face it, sometimes cooking on the week nights is a real drag. There's too much to do -- rush home from work, pick up the kids at school, homework, household chores... the list seomtimes feels endless.
Let's face it, sometimes cooking on the week nights is a real drag. There's too much to do -- rush home from work, pick up the kids at school, homework, household chores... the list seomtimes feels endless.On those crazy nights I like to dress up veggie convenience food for a tastey quick dinner. Pre-packaged grain mixes are a great place to start. One of my favorite combinations is Thai rice paired with pan seared tofu and topped with green onions, cilantro, Thai basil, chili sauce and a squeeze of fresh lime juice (see photo). You might like Spanish rice topped with pinto beans, diced onions and hot sauce or even a 7-grain pilaf with tempeh. The combinations are endless -- and dinner can be on the table in 30 minutes without much prep work at all. Pick up some boxed mixes and store them in your pantry for your next wild night!
Wednesday, June 21, 2006
Veggie Hero: Jennifer McCann
 Jennifer McCann is better known as "Jennifer Shmoo," the supermom who has inspired countless readers with her wildly popular blog, "Vegan Lunch Box." Jennifer and her family live in Kennewick, Washington.
Jennifer McCann is better known as "Jennifer Shmoo," the supermom who has inspired countless readers with her wildly popular blog, "Vegan Lunch Box." Jennifer and her family live in Kennewick, Washington.Jennifer was gracious enough to be quizzed as New Heritage Cooking's first "Veggie Hero." Thanks, Jennifer!
Vegetarian or vegan?
Vegan
How long have you been veg*n?
I first became vegetarian at age 16 -- almost 20 years ago now! -- and have been vegan on and off for the past 11 years or so.
What inspired you to go veg?
My first inspiration was reading my mom's old copy of "Laurel's Kitchen." The book's dedication to a “glossy black calf on its way to the slaughterhouse” made the decision an easy one.
What's your best story of trying to find veg food?
It would have to be the time my mother went to a local Mexican restaurant. She pointed to a soup she had never heard of. "Does this have any meat in it?" she asked. The waiter shook his head. "No, no meat." So she happily ordered the menudo soup and was quite shocked when the waiter returned with a big bowl of tripe.
How do you handle family holiday dinners?
First, inspire most of your family to go vegan (so far my son, mother, brother, and sister-in-law have made the leap). Once you outnumber the omnis, family dinners aren't so difficult.
What's your favorite veg food?
Guess!
Do you have a favorite veg book?
"Dominion: The Power of Man, the Suffering of Animals, and the Call to Mercy" by Matthew Scully
Tofu or tempeh?
Mmm, smoky marinated tempeh!
What did you have for breakfast today?
This morning I made homemade almond milk and blended it with a banana, an orange, dates, and vanilla.
In the News: Concentrated Animal Feeding Operations Near Schools May Pose Asthma Risk
 Newswise (06/21/06) — Children who attend school near large-scale livestock farms known as concentrated animal feeding operations (CAFOs) may be at a higher risk for asthma, according to a new study by University of Iowa researchers.
Newswise (06/21/06) — Children who attend school near large-scale livestock farms known as concentrated animal feeding operations (CAFOs) may be at a higher risk for asthma, according to a new study by University of Iowa researchers.The study, led by Joel Kline, M.D., professor of internal medicine in the UI Roy J. and Lucille A. Carver College of Medicine, appears in the June issue of Chest, the peer-reviewed journal of the American College of Chest Physicians.
"Previous research has shown increased rates of asthma among children living in rural areas of Iowa and the United States," said Kline, who also is deputy director of the Environmental Health Sciences Research Center (EHSRC) in the UI College of Public Health, which helped fund the study. "Given that CAFOs release inflammatory substances that can affect the health of workers at these facilities and the air quality of nearby communities, we were interested in whether there was a connection between CAFOs and increased rates of asthma among kids in rural areas."
Researchers surveyed the parents of kindergarten through fifth-grade students attending two Iowa elementary schools to compare the prevalence of asthma among students. The "study" school was located a half-mile from a CAFO in northeast Iowa; the "control" school was in east-central Iowa, more than 10 miles away from any CAFO (generally classified as a livestock facility that houses more than 3,500 animals). Sixty-one participants responded from the study school, and 248 participants responded from the control school.
Study results indicated a significant difference in the prevalence of physician-diagnosed asthma between the two schools: 12 children (19.7 percent) from the study school located near a CAFO and 18 children (7.3 percent) from the control school. The overall rate of physician-diagnosed asthma reported for Iowa is around 6.7 percent, the study authors noted.
Using the broadest definition of asthma (physician diagnosis, asthma-like symptoms or asthma medication use) the prevalence rate was 24.6 percent at the study school, compared to 11.7 percent at the control school.
Although results showed that children in the study school located near a CAFO were more likely to have a parent who smoked, which is a risk factor for asthma, the significance of parental smoking diminished when analyzed with other variables such as pet ownership, age and residence in a rural area or on a farm.
Kline stressed caution in considering the study results showing the difference in asthma diagnoses between the two schools. "Since different physicians were diagnosing asthma among the two groups, it's possible that one group may have been more or less likely to receive an asthma diagnosis for similar symptoms," he said.
What the study suggests, he added, is more research on the health effects of CAFOs.
"This is such a trigger issue in Iowa and other agricultural states, so we need to look at these results with caution," Kline said. "More study is needed on the effect of these environments on the community, not just on workers at these facilities or people who are more directly exposed."
Co-author on the Chest article was Sigurdur Sigurdarson, M.D., at the Research Center for Occupational Health and Working Life at the University of Iceland, who received his training at the UI.
In addition to the EHSRC in the UI College of Public Health, the study was supported by a grant from the National Institutes of Health.
Monday, June 19, 2006
In the News: Vegetables May Reduce Hardening of Arteries
 Newswise (06/19/06) — New research suggests one reason vegetables may be so good for us – a study in mice found that a mixture of five common vegetables reduced hardening of the arteries by 38 percent compared to animals eating a non-vegetable diet. Conducted by Wake Forest University School of Medicine, the research is reported in the current issue of the Journal of Nutrition.
Newswise (06/19/06) — New research suggests one reason vegetables may be so good for us – a study in mice found that a mixture of five common vegetables reduced hardening of the arteries by 38 percent compared to animals eating a non-vegetable diet. Conducted by Wake Forest University School of Medicine, the research is reported in the current issue of the Journal of Nutrition.“While everyone knows that eating more vegetables is supposed to be good for you, no one had shown before that it can actually inhibit the development of atherosclerosis,” said Michael Adams, D.V.M., lead researcher. “This suggests how a diet high in vegetables may help prevent heart attacks and strokes.”
The study used specially bred mice that rapidly develop atherosclerosis, the formation on blood vessel walls of fatty plaques that eventually protrude into the vessel’s opening and can reduce blood flow. The mice have elevated low-density lipoprotein ( LDL), or “bad” cholesterol, which is also a risk factor for atherosclerosis in humans.
Half of the mice in the study were fed a vegetable-free diet and half got 30 percent of their calories from a mixture of freeze-dried broccoli, green beans, corn, peas and carrots. These five vegetables are among the top-10 vegetables in the United States based on frequency of consumption.
After 16 weeks, the researchers measured two forms of cholesterol to estimate the extent of atherosclerosis. In mice that were fed the vegetable diet, researchers found that plaques in the vessel were 38 percent smaller than those in the mice fed vegetable-free diets. There were also modest improvements in body weight and cholesterol levels in the blood.
The estimates of atherosclerosis extent involved measuring free and ester cholesterol, two forms that accumulate in plaques as they develop. The rate of this accumulation has been found to be highly predictive of the actual amount of plaque present in the vessels.
Adams said it is not clear exactly how the high-vegetable diet influenced the development of plaques in the artery walls.
“Although the pathways involved remain uncertain, the results indicate that a diet rich in green and yellow vegetables inhibits the development of hardening of the arteries and may reduce the risk of heart disease,” said Adams.
He said that a 37 percent reduction in a certain marker of inflammation in mice suggests that vegetable consumption may inhibit inflammatory activity.
“It is well known that atherosclerosis progression is intimately linked with inflammation in the arteries,” Adams said. “Our results, combined with other studies, support the idea that increased vegetable consumption inhibits atherosclerosis progression through antioxidant and anti-inflammatory pathways.”
Numerous studies in humans have shown that a high-vegetable diet is associated with a reduced risk of cardiovascular disease, as well as with reductions in blood pressure and increases in “good” cholesterol. This is believed to be the first study to address the effect of increased vegetable consumption on the development or progression of atherosclerosis.
Despite compelling evidence supporting the health benefits of increased vegetable consumption, intake remains low, Adams said. The mean consumption is 3.2 servings per days, with about 40 percent coming from starchy vegetables such as potatoes.
The research was funded by the General Mills Company, which supplied the freeze-dried vegetables.
Co-researchers were Deborah Golden, B.S., Haiying Chen, Ph.D., Thomas Register, Ph.D., all with Wake Forest, and Eric T. Gugger, Ph.D., with the Bell Institute of Health and Nutrition, General Mills Company. The cholesterol analysis was performed by the Core Lipoprotein Laboratory of the Department of Pathology/Lipid Sciences at Wake Forest.
Sunday, June 18, 2006
In the News: New Strain of Mad Cow Disease not Tied to Feed
 By Elizabeth Weise, USA TODAY
By Elizabeth Weise, USA TODAYUpdated 6/18/2006 10:19 PM ET
The discovery of a new strain of mad cow disease that may strike spontaneously rather than through contaminated feed could mean that it will be impossible to completely stamp out the brain-destroying illness in cattle.
The only two cases of mad cow in U.S.-born cattle, found in Texas and Alabama, were a different form of the disease than the strain commonly found in Europe, French prion researcher Thierry Baron told scientists at a meeting in London in May.
Baron believes it is likely that the two U.S. cases — and at least five others found in France, Italy and Germany — occurred in a way that is strongly reminiscent of the most common human form of the disease, which is also not blamed on a contaminant. More research is necessary to know for certain, Baron said in an e-mail sent last week to USA TODAY.
If it can appear out of thin air to infect cattle as it does humans, "we may never be able to get rid of the disease," says Jean-Philippe Deslys, central coordinator of NeuroPrion, the network that coordinates European prion researchers.
Mad cow disease is known to scientists as bovine spongiform encephalopathy, or BSE. It is caused by infectious, misfolded proteins called prions. For most of the past decade, officials have focused their prevention efforts on banning the use of feed contaminated with infected cattle parts, believed to be the primary conduit of the disease.
Creutzfeldt-Jakob Disease (CJD) is the most common human form of prion disease. In almost 90% of U.S. cases, the prions spontaneously appear in the brain of CJD victims. About one in 1 million people, generally after age 60, are struck with the disease each year. Another 5% to 10% of CJD cases are tied to a genetic mutation.
There is no cure.
A similar but different disease is variant Creutzfeldt-Jakob, which people get from eating BSE-infected cattle. No one has acquired variant CJD in the USA; worldwide it has killed about 150 people.
Baron is quick to point out that it's not known if the spontaneously occurring form of mad cow can be transmitted by eating infected tissue.
Caroline Smith DeWaal, food safety director at the Center for Science in the Public Interest in Washington, D.C., says it's too early to say if this new strain is spontaneous. "But it does mean that ensuring that high-risk cattle material stays out of both human and animal cattle feed is essential," she says.
John Clifford, chief veterinarian of the U.S. Department of Agriculture, says feed bans across the globe have done an excellent job of stopping the transmission of mad cow. To him, what's most telling is that the number of cases is declining in cattle worldwide, as is the number of cases of variant CJD.
That's "a good indication that we're doing the right thing in control and eradication of this disease," he says.
Thursday, June 08, 2006
Chana Masala
 Sometimes you just want the taste of something different. Chana masala fits that bill nicely. This wonderfully fragrant and delicious dish from India is perfect. It doesn't take long to make and the ingredients can easily be found in a large grocery store.
Sometimes you just want the taste of something different. Chana masala fits that bill nicely. This wonderfully fragrant and delicious dish from India is perfect. It doesn't take long to make and the ingredients can easily be found in a large grocery store.1 tablespoon olive oil
1 large onion, finely diced
3 cloves garlic, minced
½ jalapeno pepper, seeded and very finely diced
1 teaspoon ground cumin
1 15 oz. can crushed canned tomatoes
2 15 oz. cans of chickpeas, drained and rinsed
1 teaspoon garam masala
1 teaspoon sea salt
¼ cup fresh cilantro, chopped
1. Heat oil in a large skillet over medium-high heat. Add onions and cook until they begin to brown. Add garlic, jalapeno and cumin. Cook 1 minute more.
2. Add tomatoes, chickpeas, garam masala and sea salt. Reduce heat to low, and simmer 10 minutes.
3. Stir in cilantro.
4. Serve over hot basmati rice.
Tuesday, June 06, 2006
The Importance of Vitamin B12
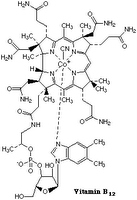 By Dr. Amy Joy Lanou
By Dr. Amy Joy LanouTo me vitamin B12 is one of the most interesting vitamins.
Marginal vitamin B12 deficiency is fairly common, largely not because of insufficient intake, but because it requires a complex set of circumstances to be absorbed. In order to be absorbed, one's stomach needs to be sufficiently acidic and the body needs to make a substance called intrinsic factor. In the presence of an acidic environment in the stomach, intrinsic factor complexes with vitamin B12. Intrinsic factor is required for vitamin B12 to be absorbed in the intestines. Acid is required for intrinsic factor and B12 to complex together. Elders and people with ulcers caused by bacterial overgrowth in the stomach often do not have sufficiently acidic environment for the vitamin B12 to complex with intrinsic factor. Also some individuals do not make enough intrinsic factor. In both of these cases, adding more B12 through the diet or supplements will not solve the problem. This is when B12 shots directly into the tissue become necessary (bypassing the absorption step). Individuals with bacterial overgrowth in their stomachs and duodenums can often be treated (and in most cases should be) when this happens, the stomach can often return to its normal acidic state, and B12 shots will not be necessary.
Frank deficiency is a real concern because it can cause irreversible nerve damage. Because vitamin B12 is needed for the breakdown of homocysteine (an independent risk factor for coronary heart disease), even marginal deficiency should be avoided.
Most omnivores do not need to worry about consuming enough vitamin B12 -- there is plenty in animal products to meet one's needs. And humans generally store up to about a five-year supply in the body which makes thinking about this vitamin more relaxed!
Vitamin B12 is made by bacteria in the guts of animal (including humans although we don't get much that way because we make it in the large bowel and its not absorbed well from there) and in most animals is then absorbed and incorporated into the tissues and secretions (meat, milk, etc.).
I do recommend fortified foods or supplements for vegans. In fact, it is really important for vegans to pay attention to getting a fairly regular supply of B12. Vegetarians consuming three daily servings of dairy products probably do not need to supplement, but it wouldn't hurt.
Good vegan sources include nutritional yeast, fortified cereals, fortified veggie meats, fortified soy and rice milks, and supplements. Any vitamin source containing B12 is fine. I prefer a high dose B12 only supplement that is used weekly rather than having to remember to take something daily. I like the sublingual or chewable versions because some absorption can happen through the mouth. The body will not absorb more than will be beneficial and it does store a fairly good supply so the periodic use of a supplement along with regular use of a fortified food source is more than sufficient.
-- Dr. Lanou is a Senior Nutrition Scientist for the Physicians Committee for Responsible Medicine and Assistant Professor of Health & Wellness University of North Carolina at Asheville. Article reprinted with her permission.
Sunday, June 04, 2006
Simple Summer Squash Saute
 Tender, young summer squash is beginning to be available at my local farmer's market. It's a wonderfully quick cooking vegetable that makes a nice side dish for a sandwich. Perfect for a night when you don't really feel like cooking but want something fresh.
Tender, young summer squash is beginning to be available at my local farmer's market. It's a wonderfully quick cooking vegetable that makes a nice side dish for a sandwich. Perfect for a night when you don't really feel like cooking but want something fresh.2 medium summer squash, quartered and sliced
1/2 medium onion, sliced
2 teaspoons extra virgin olive oil
1/4 teaspoon fine sea salt
1/2 teaspoon dried oregano
1. Heat olive oil in a large skillet over medium heat until it begins to shimmer -- about one minute.
2. Add all other ingredients. Cook 7-10 minutes, stirring occassionally, until squash is tender.
Saturday, June 03, 2006
Pancakes
 Pancakes make a wonderful weekend breakfast. These pancakes are packed with nutrition and taste great, too! I worked on this recipe for months, getting it just right. The combination of wheat flour and cornmeal is the secret!
Pancakes make a wonderful weekend breakfast. These pancakes are packed with nutrition and taste great, too! I worked on this recipe for months, getting it just right. The combination of wheat flour and cornmeal is the secret!¾ cup unbleached flour
¼ cup cornmeal
½ tablespoon ground flax seed
2 teaspoons non-aluminum baking powder
1/8 teaspoon sea salt
1 cup soymilk
1 tablespoon expeller-pressed canola oil
1 tablespoon pure maple syrup
1. In a medium bowl, whisk together flour, cornmeal, flax seed, baking powder and sea salt.
2. Add soymilk, canola oil and maple syrup. Mix until just combined.
3. Lightly spray a large skillet with cooking oil and warm over medium-high heat.
4. Measure about 1/3 cup of batter onto the hot skillet. Flip pancake when bubbles appear and burst on the upper surface, about 2 minutes. Cook for another 2 minutes or until set.
5. Serve immediately with warm maple syrup and butter.
Friday, June 02, 2006
Blueberry Streusel Coffee Cake
 On special mornings, don't you long for a celebratory breakfast? Try this wonderful Blueberry Streusel Coffee Cake. It is full of whole grains, unprocessed sugars and juicy blueberries.
On special mornings, don't you long for a celebratory breakfast? Try this wonderful Blueberry Streusel Coffee Cake. It is full of whole grains, unprocessed sugars and juicy blueberries.Cake
¾ cup whole wheat pastry flour
¾ cup unbleached white flour
2 ¼ teaspoon aluminum-free baking powder
¼ teaspoon sea salt
¼ cup expeller-pressed canola oil
½ cup pure maple syrup
¾ cup vanilla soymilk
1 teaspoons vanilla
1 cup fresh or frozen blueberries
Streusel
¼ cup milled cane sugar
¼ cup rolled oats
¼ cup chopped pecans
2 tablespoons whole wheat pastry flour
½ teaspoon cinnamon
¼ teaspoon nutmeg
2 tablespoons expeller-pressed canola oil
1. Preheat oven to 350 degrees. Lightly grease a 10-inch spring form pan. Set aside.
2. Begin by preparing streusel topping. In a small bowl, combine sugar, oats, pecans, flour, cinnamon and nutmeg. Cut in oil and mix until mixture is crumbly. Set aside.
3. Next prepare the cake batter. In a medium mixing bowl, combine flours, baking powder and sea salt. Remove 1 tablespoon of flour mixture, sprinkle over blueberries and toss to coat.
4. Add oil, maple syrup, soymilk and vanilla to flour mixture. Mix until just combined. Turn in coated blueberries.
4. Pour batter into prepared cake pan. Top evenly with streusel.
5. Bake cake for 40-45 minutes or until probe inserted into the center comes out clean.
6. Cool on a wire rack for 10-15 minutes. Remove from pan and continue cooling.
7. Serve warm. Cover any leftovers.
Thursday, June 01, 2006
New Heritage Cooking
 My love affair with animals began at an early age. When I was four years old, my parents conspired with my grandfather and great uncle -- both farmers -- to give me and my sister each a baby lamb for Easter. You simply cannot imagine our delight on Easter morning! We were smitten! I named my lamb Snow White and my sister named hers Flour.
My love affair with animals began at an early age. When I was four years old, my parents conspired with my grandfather and great uncle -- both farmers -- to give me and my sister each a baby lamb for Easter. You simply cannot imagine our delight on Easter morning! We were smitten! I named my lamb Snow White and my sister named hers Flour.It was a cool spring and the lambs stayed inside with us. I can remember the lambs sleeping in a giant cardboard box next to the wood-burning stove and even sitting with us while we watched TV!
Eventually, the lambs moved outside and then back to my great uncle’s farm. I had a hard time understanding what happened when later that year my parents said that our lambs had gone “to market.”
As I got older, I began to better understand the cycle of life on a farm and how food arrives on the dinner table. My family had an orchard, an arbor and a large garden. My mother baked bread several times per week and made nearly everything else from scratch. We raised our own animals for food -- rabbits, ducks, chickens and turkeys. My parents also butchered hogs and even rendered the lard in a big, black cauldron over an open fire.
We rounded out our diet with wildcrafted food. I remember mushroom hunting in the spring, picking wild berries in the summer, and digging sassafras roots in the winter. My father, a skilled hunter and angler, provided the table with deer, squirrel, goose, duck, pheasant, crayfish, frog legs, turtle, fish and other wild game.
Despite the tranquility of such a natural life, I was deeply troubled by our relationship to the animals. Part of my daily chores included feeding the ducks, chickens and turkeys and I grew very fond of them. I would often spend my summer days under the shade of the plum trees visiting my feathered friends. I especially enjoyed two turkeys, Tom and Betty. When I sat in the grass of their open-air pen, Tom and Betty settled in on either side of me, resting their heads on my knees, waiting for strokes across their glossy backs. They loved to eat treats straight from my hand and would sit for hours listening as I read story books aloud to them. They adored human companionship so much that they would even follow me around the farm when let out of their pen.
Eventually, summer turned to fall -- butchering time. Tom and Betty became the centerpieces of our family's Thanksgiving and Christmas dinners. I was devastated. On the morning of Thanksgiving I sat in my room and cried for my lost friends -- and decided to never eat turkey again.
Soon I swore off chicken, as well. What began as a simple 4-H project focused on chicken husbandry turned into a personal relationship with my little flock of six chickens. I was absolutely crushed at butchering time. Each chicken had a name! How could we dine on them?!
Though I had never met a vegetarian in our small rural community, I knew that a more compassionate way of living was the life for me. At age 18, I checked the one lone vegetarian book, “Laurel’s Kitchen,” out of our county library. I read the book cover to cover and overnight became a vegetarian. Now, 16 years later, I've not once regretted my decision to spare the lives of countless animals.
On the farm I learned more than compassion – my mother and grandmother also taught me how to cook and bake. Both were masters in the kitchen – earning the highest praise from friends and family and even taking home top prizes at county fairs. So it is no surprise that they placed a true value on these skills and taught me well.
Unfortunately, many people today choose not to cook, have forgotten how or never learned in the first place. It's surprising that even many vegans and vegetarians choose to warm up packaged food or eat out rather than cooking at home. It is time to heal this rift and reclaim the wisdom to honestly nourish ourselves.
"New Heritage Cooking" brings us back to the kitchen, armed with a new paradigm of compassionate eating that is more beneficial to our health, the animals and the Earth. It is a way to deeply reconnect to traditional home-style cooking, while using new products and techniques to bring truly comforting and compassionate food to the table.
Subscribe to:
Comments (Atom)



